How To Engage Your Core - Essential Exercises for Over 60
As we age, it becomes increasingly important to maintain a strong and stable core, which is essential for overall functional fitness and everyday activities.
A strong core not only improves posture and balance but also supports daily activities and reduces the risk of injuries.
A simple technique to engage the core is to "draw the belly button to the spine."
Building a Solid Foundation: Core Strengthening TipS fOR SENIORS
The core is composed of a complex group of muscles that work together to provide stability, support, and movement for the entire body.
Core Muscles
The Deeper Core Muscles
The primary muscles of the core include the rectus abdominis, obliques (internal and external), transverse abdominis, and erector spinae.
The rectus abdominis, commonly known as the "six-pack" muscles, run vertically along the front of the abdomen and help flex the spine.
The obliques, located on the sides of the abdomen, aid in rotation and lateral flexion of the trunk.
The erector spinae muscles run along the length of the spine and assist in extending the back.
Lastly, the transverse abdominis (TrA) is a deep muscle that wraps around the torso like a corset and plays a crucial role in core stability and spinal support. We will be focusing more so on this muscle today.
As we age, it becomes increasingly important to maintain a strong and stable core, which is essential for overall functional fitness and everyday activities.
A strong core not only improves posture and balance but also supports daily activities and reduces the risk of injuries.
A simple technique to engage the core is to "draw the belly button to the spine."
Drawing the Belly Button to the Spine:
This is a cue frequently used to activate the deep abdominal muscles, particularly the transverse abdominis.
To engage your core using this technique, follow these steps:
a. Begin by sitting or standing tall with good posture. Or alternatively, you can do this lying with your knees bent and your feet flat on the floor
b. Find your neutral spine position - Ensure you are not slouched or your back is not over-arched.
c. Now gently draw your belly button in towards your spine.
d. Breath Naturally - Maintain a steady, controlled breath while keeping your abdominal muscles engaged.
d. Hold this position for a few seconds and release.
e. Repeat the exercise for a certain amount of repetitions, gradually increasing the duration of the hold.
For a video on this technique, click here below (or HERE):
IS THIS THE SAME AS SUCKING IN THE STOMACH?
"Sucking in your stomach" typically refers to the act of pulling in or tightening the abdominal muscles superficially, often for aesthetic purposes or to create a slimmer appearance.
This action primarily engages the external abdominal muscles, such as the rectus abdominis and external obliques, without necessarily activating the deeper core muscles.
On the other hand, "bringing your belly button to your backbone" or "drawing the belly button to the spine" is used to engage the deep core muscles, specifically the transverse abdominis. You’re bringing your muscles in towards your spine.
This technique emphasises activating the muscles that lie deeper within the abdomen, closer to the spine.
It provides greater stability and support to the core, promoting better posture and functional movement.
While both actions involve some level of core engagement, the latter technique of bringing the belly button to the spine focuses on activating the deep core muscles, which offer more substantial benefits for overall core strength and stability.
Other Terms for Core Engagement:
Drawing the belly button to the spine is a popular cue to engage the core.
However, you have most probably heard other terms and techniques to help you to engage the core effectively.
Here are some alternatives:
1. Core Compression:
This involves contracting the muscles around the abdomen, including the rectus abdominis, obliques, and transverse abdominis.
Imagine compressing your midsection inward as if you were wearing a tight corset. This cue emphasizes activating the entire core area.
2. Hollowing the Stomach:
Hollowing the stomach refers to pulling the abdominal muscles inward while maintaining a natural curve in the lower back. Imagine hollowing out your belly, drawing it towards your spine without holding your breath or squeezing too tightly.
3. Bracing:
Bracing involves tensing the abdominal muscles as if you were preparing to take a punch. This technique provides stability and support to the core, similar to how a brace supports a structure.
Core-Strengthening Exercises for Seniors:
Now that you are familiar with various ways engage the core, for core strengthening exercise videos for seniors (including seated videos), click HERE.
Engaging the core is an important exercise to maintain stability, balance, and overall functional fitness and these techniques above can be practiced anywhere!
Whether you prefer the cue "drawing the belly button to the spine" or other terms such as core compression, hollowing the stomach, or bracing, the goal is to activate and strengthen the deep core muscles.
By incorporating core-strengthening exercises into your fitness routine, you can improve your posture, enhance balance, and enjoy an active lifestyle with reduced risk of injury.
Have you heard these cues for strengthening your core? Maybe you have heard others? If so, let me know below!
All About Spinal Stenosis & What You Can Do About It!
The word “stenosis” is used in medicine to describe a narrowing of a passage of the body.
In spinal stenosis, as you may have already guessed, the narrowing is of an area of the spine.
The symptoms associated with this condition can make daily life difficult. However, it’s important to understand that chronic pain (and other chronic symptoms) are usually caused by multiple factors. NOT solely from the diagnosed issue itself (in this case, spinal stenosis).
There are also many effective treatments available.
By taking the right steps and seeking the right Health Professionals, YOU CAN GET RELIEF!
Relieving Spinal Stenosis
(Includes Best Exercises For Spinal StenosiS)
The word “stenosis” is used in medicine to describe a narrowing of a passage of the body.
Spinal stenosis, as you may have already guessed, is the narrowing of an area of the spine.
Spinal stenosis is a condition that can more commonly affect those over 60. It can lead to various symptoms, including lower back pain, weakness in the legs or arms, numbness in the buttocks or legs, or balance and mobility issues.
The symptoms associated with this condition can make daily life difficult. However, there are many effective treatments available and by taking the right steps, YOU CAN GET RELIEF!
In this article, we are going to look at spinal stenosis and what you can do about it! (including exercises, with an exercise video that will help).
WHAT’S COVERED IN THIS ARTICLE:
Note: Do not self-diagnose based on the information in this article. If you are experiencing any of the symptoms discussed in this article, make sure you see your Doctor or Physiotherapist before coming to any conclusions.
UNDERSTANDING SPINAL STENOSIS (TO BRING RELIEF)
ABOUT OUR SPINE
To better understand spinal stenosis, a little knowledge of the spine is needed. Let’s take a look at that now.
The Regions of the Spine
Our spine is a strong structure that supports our upper body. It keeps us upright and standing straight.
It’s also a flexible structure that allows certain movements. It can bend forward (flexion), bend backward (extension), twist to each side (rotation) and bend to each side (lateral flexion).
Our spine comprises 29 smaller bones that run from our neck to our pelvis (to the tail bone).
There are seven bones in the cervical region (the neck), twelve in the thoracic region (the upper back), five in the lumbar region (the lower back) and five bones, which are fused (and don’t move), in the sacral region (the pelvis).
These bones are called vertebra or vertebrae (plural).
Between each of our vertebrae are intervertebral discs which act as little cushions and provide shock absorption.
Vertebrae, Intervertebral discs and spinal cord
The intervertebral discs also allow our spine to move.
In the middle of our spine, a column of nerves runs through these bones. This column of nerves is our spinal cord. The space in which the spinal cord sits is known as the foramen.
The spinal cord is quite delicate and it is protected by the surrounding vertebral bone and other tissues.
Nerves of the spinal cord branch off at every level of the vertebrae to allow signals from the brain to reach the rest of the body.
ABOUT SPINAL STENOSIS
Throughout life, changes to the spine can occur for various reasons.
These changes can cause the spaces the spinal nerves pass through to become narrowed (aka spinal stenosis).
Any narrowing where the nerves pass through can pinch the nerves leading to pain and neurological symptoms that can affect walking, balance and sensation, and cause paralysis.
Spinal stenosis can happen in any part of the spine but most commonly occurs in the lumbar and cervical regions.
Lumbar stenosis is the most common type of spinal stenosis.
CAUSES OF SPINAL STENOSIS
Changes to the spine that cause spinal stenosis are:
OSTEOARTHRITIS
Over the years, our joints experience wear and tear, otherwise known as osteoarthritis. Osteoarthritis is the most common cause of spinal stenosis.
Osteoarthritis can cause the spaces the nerves pass through (the foramen) to become narrowed.
The wear and tear can also lead to abnormal bone growth, called osteophytes or bone spurs, which can cause narrowing of the foramen and put pressure on the nerves.
INTERVERTEBRAL DISC ISSUES
Additionally, as we get older, the discs between our vertebrae lose height and become dehydrated (this is why we lose height as we age).
As the discs become thinner, there is now increased pressure on the spinal joints, and it can also lead to narrowing of the foramen.
The intervertebral discs can also bulge, pushing into the spinal canal, leading to spinal stenosis.
LIGAMENT THICKENING
Another cause of spinal stenosis is a thickening of the spine's ligaments, caused by osteoarthritis and inflammation. [1]
SYMPTOMS OF SPINAL STENOSIS
With spinal stenosis, the symptoms vary between each person.
The most common symptom is pain radiating down the legs. This pain is usually felt in both legs but can occur in only one.
The pain is usually aggravated when hyper-extending the back (leaning/bending backwards). See diagram below.
Position of most pain - extending.
Additionally, prolonged walking or standing also commonly increase the symptoms.
Other common symptoms of spinal stenosis are numbness and weakness in the legs, which can lead to balance and mobility issues.
On the other hand, certain positions relieve pain, which is characteristic of spinal stenosis.
Bending forward relieves the pain (e.g. leaning forward on a table when standing, or a shopping trolley, or walking aid, when walking).
HOW IS SPINAL STENOSIS DIAGNOSED
If you are experiencing any symptoms discussed above, see your doctor or Physiotherapist for an appropriate assessment and diagnosis.
Your doctor may order medical images/scans (X-ray and/or MRI).
As mentioned at the beginning of this article, there is no direct link between the severity of stenosis seen on medical imaging and symptoms. One may have severe stenosis on scans and no pain, and another can have mild stenosis on scans and severe pain.
How is this possible? Because scans CANNOT tell you what is causing your pain. Pain is caused by a variety of reasons.
Scans can, however, give an idea of what is going on in your back, which helps with recovery.
Therefore you mustn't get too caught up in the results of your scans or the diagnosis of spinal stenosis. Instead, turn your attention to applying what's required to remedy your pain.
I cover medical imaging and beliefs around pain in detail in my articles on chronic pain. You can find all these articles HERE. In Part 1 of my Pain Series articles - Pain is More than Meets the Eye we look at pain from a different angle and Part 2: The Real Causes of Pain - I demonstrate, backed with studies, that what is identified on scans is not the sole cause of your pain.
Once you have an idea of what is causing your pain, your doctor will help you decide on the appropriate treatment. A conservative, exercise and lifestyle-based approach is usually the first line of treatment for spinal stenosis.
Now let's get to what you can do to help bring relief from spinal stenosis.
GETTING RELIEF FROM SPINAL STENOSIS
We have now covered that multiple factors contribute to pain and other symptoms in spinal stenosis and other chronic, painful conditions.
I discuss these factors that usually contribute to chronic pain and other symptoms in more detail in my article: “Overcoming Pain - Empty Your Cup” - (click to read).
When symptoms from spinal stenosis are increased, the best solution is to rest and avoid what is aggravating them.
At these times, management techniques can help also. These techniques include analgesia (speak to your doctor about this), heat packs, heat rubs/creams, cryotherapy (ice), herbal remedies, TENs (Transcutaneous Electrical Stimulation), ultrasound, acupuncture, cupping, stretching, amongst many others.
Rest and analgesia are not long term solutions and will eventually lead to further issues.
Exercise, along with other lifestyle changes, on the other hand, are long term solutions!
A gradual return to movement and activity is necessary as symptoms improve.
Additionally, other factors such as changing your views surrounding pain, shifting your focus on leading a healthier life, reducing stress, sleeping better, eating healthily, getting moving/exercising and doing specific exercises (covered in the next section) will help you overcome your symptoms.
I discuss lifestyle changes in more detail in my article “Overcoming Pain - Empty Your Cup Article”. And, In Part 4 of the Pain Series articles, “Overcoming your pain”, make sure to check them out.
The articles I have linked to above will give you new ways to think about your pain and solutions to begin living a healthier life and help bring relief from your spinal stenosis.
There are also many health professionals and clinics that can help you with your condition. So speak to your doctor or Physiotherapist or seek the right Health Professional for you who can help.
Being in pain/suffering is NOT a normal part of aging. There are many things you can do to help bring relief. You do not have to put up with the symptoms of spinal stenosis.
EXERCISING TO IMPROVE SPINAL STENOSIS
When in pain, the urge may be to avoid exercise altogether. In the beginning or during a flare-up of symptoms, this is ok.
However, exercise and movement are vital to manage and help overcome spinal stenosis (and any painful, chronic condition). This will ensure you remain moving well and your muscles and joints stay strong and flexible.
I recommend seeing a Physiotherapist if you are experiencing symptoms from spinal stenosis (or any back pain for that matter) as they can determine what physical issues could be contributing to your pain and develop an individualised exercise program for you.
They will also teach you specific exercises, ensure you are doing them correctly, keep track of your progress and modify your exercises where need be.
EXERCISES THAT MAY AGGRAVATE SPINAL STENOSIS
Avoiding any body movements can lead to further issues - such as increased stiffness and weakness.
However, with all painful conditions, there may be specific movements at times that will aggravate your pain, especially when symptoms are increased.
As discussed earlier, extension movements, movements leaning backwards, are common positions that cause pain with spinal stenosis.
I am demonstrating some movements in the extension position in the pictures below.
Seated lumbar extension
An increased lumbar extension stretch - Hyperextension
On the other hand, flexion movements (covered in the next section) will help ease your symptoms of spinal stenosis.
Also, stretches in standing may increase symptoms. Seated or lying stretches may be better.
Other activities that may aggravate symptoms of spinal stenosis are strengthening exercises (free weights), other high-impact exercises (for example, dancing, jogging or certain sports) and long walks (longer distances and time).
Although you may need to avoid, limit or modify certain exercises or activities initially, it does not mean you have to avoid them for good. These activities and exercises mentioned above bring many health benefits.
Free weights can be an excellent tool for a stronger body and help with back pain, provided they are performed correctly, and you have a clearance from your doctor or Physiotherapist.
Walking is another excellent form of exercise, and exercise everyone should be doing as they are able. Start with shorter, gentle walks before progressing. For more on this, make sure to check out my article on walking HERE.
It is important to have a healthy outlook on your pain. Aim to return to your previous levels of activity, and then eventually moving beyond that and doing more types of exercise as your symptoms and movement improve over time.
EXERCISE CHOICES FOR SPINAL STENOSIS
There are always alternate exercise options if you cannot do certain activities or exercise due to your pain or other symptoms.
One of those options is swimming or exercising in water (hydrotherapy).
Although swimming puts you in a more extended position, most people experience less or even no symptoms due to the non-weight bearing, low impact nature.
Swimming allows you to exercise your body with decreased stress/impact.
Additionally, if you are having difficulty doing exercises due to pain, exercising in water (known as hydrotherapy) can allow you to exercise your body without increasing symptoms due to your increased buoyancy (or decreased weight-bearing) in the water.
Furthermore, heated pools can help relax muscles and reduce pain, which will make the exercises more manageable and allow a greater range of movement compared to when out of the water, leading to more benefits.
After some time exercising in water, land-based exercise will begin feeling easier.
Other types of exercise that may help with your pain include smaller walks (building this up over time), yoga, pilates, or riding a stationary bike.
BEST EXERCISES FOR SPINAL STENOSIS
5 BEST EXERCISES FOR LUMBAR STENOSIS
Here are the best exercises you can do to help bring relief from your symptoms of spinal stenosis. There is an exercise video in the next section, which you can follow. The video will make it all easier.
If you have trouble getting up or down off the floor, I recommend doing these exercises on a firm bed.
Aim to complete these exercises once per day.
Go at your own pace and repeat for the repetitions stated below.
As you continue with the exercises, gradually increase the repetitions, time and sets over time.
Note: Remember to consult your Doctor or Physiotherapist to ensure these exercises are appropriate for you. If these exercises cause an increase in pain or other symptoms, stop the exercise and make sure to speak to your Doctor or Physiotherapist.
1. KNEE TO CHEST FLEXION STRETCH (DOUBLE)
How To:
Lie on your back, with your body comfortable and relaxed.
Bring both your knees to your chest and hug them, keeping your spine relaxed throughout.
Hold this position for 10 seconds and then slowly lower the legs.
Repeat 5 times.
2. SINGLE KNEE TO CHEST FLEXION STRETCH
How To:
Similar to the exercises above, this time drawing one leg up at a time.
Lie on your back, with your body comfortable and relaxed and legs extended.
Bring one knee to your chest and then bring it closer to your chest by placing your hands either at the back of the thigh or just below the knee.
Hold this position for 5 seconds and then slowly lower the leg, and alternate legs.
Repeat 5 times each side.
3. LUMBAR ROTATIONS
How To:
Lie on your back, with your arms by your side and with your knees bent at 90 degrees,.
To begin keep both feet flat against the floor.
Slowly rotate the knees to the left side as far as you can, then slowly rotate the knees to the right side.
The soles of your feet will lift off the ground when doing this exercise.
Repeat this for 5 repetitions each side.
4. BRIDGE
How To:
Lie on your back with knees bent at 90 degrees , your arms by your side and palms against the floor.
Squeeze your buttocks and raise the hips off the ground to bring the torso into a straight diagonal line.
Hold this position for 5 seconds then slowly lower your bottom back to the ground.
Repeat 5 times.
5. SEATED LUMBAR FLEXION
How To:
Sit in a firm chair with both feet on the floor.
Slowly bend yourself forward and reach towards the floor.
Hold the fully bent position for 5 seconds.
If you need to increase the pressure, hold your ankles and move into the stretch a little more.
After holding for 5 seconds, release and return to the full, upright seated position.
BEST EXERCISES FOR LUMBAR STENOSIS (VIDEO)
3 BEST EXERCISES FOR CERVICAL STENOSIS
Exercises for cervical spinal stenosis also work to improve the strength and flexibility of the neck and upper back.
Here are some upper back and neck exercises for spinal stenosis.
1. BACKWARD SHOULDER ROLLS
How To:
Sitting up nice and tall in your chair with your feet flat on the ground.
Lift your shoulders up toward your ears and then roll them back and down.
Now relax into the starting position.
Repeat this rolling motion.
Complete for 10 repetitions.
2. SEATED SHOULDER SQUEEZES
How To:
Sitting upright in your chair in good posture.
While seated, draw your shoulder blades together, hold for a second or two, and then lower back to the start position
Repeat for 10 repetitions.
3. CHIN TUCKS
How To:
Sitting upright in your chair in good posture
Maintaining this upright posture retract your chin out and slowly tuck your chin all the way in.
Do not move your head up or down during this movement.
Ensure you maintain the upright seated posture
Repeat for 10 repetitions.
SOURCES
Spinal Stenosis. https://www.ncbi.nlm.nih.gov/books/NBK441989/
Easing Peripheral Neuropathy
Peripheral neuropathy is a condition that affects and damages the nerves of the peripheral nervous system, causing them to malfunction.
Symptoms of peripheral neuropathy may range from mild to severe, depending on the type of the affected nerves, as well as the gravity of the damage.
Sometimes, the symptoms occur suddenly, but in most cases, the symptoms develop gradually over a longer period.
INCLUDES Exercises for Peripheral NEUROPATHY
Over the years, having helped many patients with peripheral neuropathy experience relief from their symptoms, I have witnessed how uncomfortable this condition can be, and I want to do my bit in helping bring relief to as many as I can.
I have written this in-depth article to help bring you a better understanding of peripheral neuropathy and what you can do to ease the uncomfortable symptoms that come along with it.
I have also included an exercise program in video and pictures that you can follow to help you improve your strength and flexibility, relax your body and muscles and help reduce the symptoms.
So, let’s get into it!
This article covers the following:
WHAT IS PERIPHERAL NEUROPATHY?
Peripheral neuropathy is a condition that affects and damages the nerves of the peripheral nervous system, causing them to malfunction.
To understand this condition a little better, we’ll need to get a grasp on the function of the nervous system, and more specifically, the peripheral nervous system itself.
The nervous system of our body is made up of two major components, both the central nervous system (CNS) and the peripheral nervous system (PNS).
The central nervous system comprises the brain and the spinal cord. This part of the nervous system is the processing centre of the body.
It controls both our body’s voluntary functions (functions we consciously control) and involuntary functions (automatic functions). The CNS is responsible for interpreting information from the PNS and responding to this information.
The peripheral nervous system on the other hand, is a complex network of nerves that connects your brain and spinal cord to, as you might have guessed from the name, the peripheral areas of your body. It’s the parts of the nervous system outside the brain and spinal cord.
To put it simply, the peripheral nervous system allows your brain and spinal cord (the CNS) to communicate with your body parts (your limbs, skin, muscles, and internal organs). It communicates to your CNS, for example letting your brain know you’ve touched something hot. And it also carries messages from the CNS to different parts of your body (E.G. moving your hand off the hot item).
In the case of peripheral neuropathy, the nerves outside your brain and spinal cord are damaged leading to unpleasant symptoms usually in the lower legs and feet, or the hands.
TYPES OF PERIPHERAL NEUROPATHY
There are different kinds of peripheral neuropathy and they’re generally categorised based on the number of affected nerves. As such, we recognise mononeuropathy and polyneuropathy.
Mononeuropathy is a type of neuropathy that affects only a single peripheral nerve. The most common cause of mononeuropathy is physical injury to the affected area or prolonged pressure on the specific nerve. Mononeuropathy is often observed in patients who lead an overly sedentary lifestyle or are involved in activities that cause repetitive motions in specific areas of the body.
One such example is carpal tunnel syndrome. This condition is caused by prolonged pressure on the nerve which passes through the wrists and ends in the hands. People who work office jobs or assembly lines in factories are often affected due to the overuse of their wrists. This condition is characterised by numbness, tingling, and pain in the hands, usually in the first three fingers starting from the thumb.
Polyneuropathy, on the other hand, is a type of neuropathy that affects multiple peripheral nerves at once. Most of the cases of peripheral neuropathy are, in fact, polyneuropathies. The condition results in weakness, numbness, and burning pain, which usually starts in the hands and feet and often progresses throughout the body, affecting other areas as well.
Polyneuropathy occurs due to a multitude of reasons, although the most common form of polyneuropathy is diabetic neuropathy, generally observed in patients suffering from diabetes or those with irregular blood sugar levels.
The condition can be acute or chronic in nature.
Acute polyneuropathy is often a result of an infection or an autoimmune reaction. It occurs suddenly and poses a higher risk with more severe symptoms. Guillain-Barré syndrome is one of the most serious forms of acute polyneuropathy where the immune system attacks the nerves in the body. This disorder spreads quickly and if left untreated, it can lead to permanent damage and even paralysis.
Chronic polyneuropathy is when the neuropathy is longer lasting and is generally difficult to treat. There are different causes of this condition and some are a direct result of underlying disorders such as diabetes.
SYMPTOMS OF PERIPHERAL NEUROPATHY
Symptoms of peripheral neuropathy may range from mild to severe, depending on the type of the affected nerves, as well as the gravity of the damage.
Sometimes, the symptoms occur suddenly, but in most cases, the symptoms develop gradually over a longer period.
In certain cases, symptoms may go away on their own, without any intervention. Other cases may require medical attention, but it’s important to keep in mind that treatments are available and can greatly alleviate the symptoms of these disorders.
The symptoms of peripheral neuropathy can vary and depend on the type of damaged nerves. These types can be motor, autonomic, and sensory nerves.
Motor Nerves
Motor nerves are in charge of the muscle movements in the body. They control how we walk, how we talk and when we undertake certain actions, like holding a cup of coffee. When your motor nerves are affected you may experience symptoms such as muscle loss (atrophy), muscle weakness and spasms, coordination loss and falling. Loss of reflexes, difficulty moving your arms and legs or paralysis.
Autonomic Nerves
These nerves are responsible for bodily functions that people can't control consciously. This includes breathing, digestion, bladder function, as well as heart rate. Damaged autonomic nerves can result in nausea, vomiting, sweating, dizziness, abnormal heartbeat, as well as gastrointestinal issues.
Sensory Nerves
When you get a paper cut or burn your mouth with some scolding coffee, it’s your sensory nerves that are alerting the brain of these sensations. If the peripheral neuropathy has damaged your sensory nerves, you may experience either a heightened or a decreased sensitivity to touch. Burning, sharp or throbbing pains. Other symptoms include tingling and numbness, and decreased reflexes. Many people also report a feeling as if they are wearing tight gloves or socks.
Nerves have the responsibility to send signals to your brain. When those nerves are damaged, the signals may be interrupted or misinterpreted.
In some cases, your nerves may alert your brain of pain sensations that aren’t even there; similarly, they might not send the signals when the pain does occur.
Peripheral neuropathy can be caused by several factors and can often be a result of underlying conditions. It’s essential to determine the underlying causes to your neuropathy, as it’s important to treat the root of the problem, rather than just the symptoms.
COMMON CAUSES OF PERIPHERAL NEUROPATHY
Peripheral neuropathy isn’t caused by a single factor and it can be a result of different medical conditions, traumatic injuries, infections, alcoholism, and even certain medicines. By far the most common cause of peripheral neuropathy is diabetes.
Diabetic polyneuropathy is progressive nerve damage caused by type 1 and type 2 diabetes. Studies show that peripheral neuropathy affects nearly 50% of adults with diabetes. There is no available cure for diabetic neuropathy, but it is possible to slow the progression with certain lifestyle changes.
Aside from diabetes, several other health conditions can cause peripheral neuropathy. These conditions include:
Inherited disorders
Also called hereditary motor and sensory neuropathy, Charcot–Marie–Tooth disease (CMT) is a type of disorder that causes nerve damage, mostly in the arms and legs. It is known to be one of the most common inherited neurological disorders.
Bone marrow disorders
Certain conditions characterised by abnormal levels of protein in the blood are also known to cause peripheral neuropathy.
Autoimmune diseases
Guillain-Barre syndrome is one of the most severe types of peripheral neuropathy caused by an autoimmune disease.
Other medical conditions caused by an abnormal immune system response that are linked to neuropathy are Sjogren’s syndrome, rheumatoid arthritis, lupus, vasculitis, and chronic inflammatory demyelinating polyneuropathy (CIDP).
Infections
Peripheral neuropathy can also be a result of certain bacterial and viral infections. Lyme disease, leprosy, diphtheria, and HIV are some of the infections known to cause neuropathy.
Other diseases
Several other diseases such as kidney and liver disease, certain cancers, hypothyroidism, and connective tissue disorders are also linked to potential peripheral neuropathy.
Peripheral neuropathy can also be caused by other factors, such as:
Traumatic injuries
Physical injuries, including sports injuries, falls, automobile accidents, or complications during surgery are some of the most common causes of mononeuropathy. Such injuries can compress and stretch the nerves, or even cause them to detach from the spinal cord.
Medications
Peripheral neuropathy sometimes occurs as a side effect of certain medications. Research suggests that drug-induced peripheral neuropathy is commonly observed in chemotherapeutic agents, antimicrobials, cardiovascular drugs, psychotropic, and anticonvulsant drugs.
Toxins
Prolonged exposure to poisons and toxic substances such as lead, arsenic, thallium, and mercury can also cause neuropathy.
Vitamin deficiencies
Vitamins play a big role in regulating our nervous system. A deficiency in certain vitamins, (especially B vitamins) have been linked to a higher risk of peripheral neuropathy.
Certain studies show that patients undergoing bariatric surgery should especially pay attention to possible deficiencies in their systems.
Alcoholism
Excessive alcohol usage is also associated with neuropathy due to several risk factors.
Research shows that thiamin deficiency, malnutrition, and direct alcohol toxicity could be the main reasons behind alcoholic neuropathy.
Sometimes it’s not possible to determine the exact cause of peripheral neuropathy. When this happens, it is called idiopathic neuropathy.
TREATMENT OPTIONS FOR PERIPHERAL NEUROPATHY
Now that we’ve explained what peripheral neuropathy is, how it develops and the way it manifests itself, you’re probably wondering - is it treatable?
Unfortunately, there isn’t an easy answer to this question. Certain types of peripheral neuropathy can be effectively treated and even reversed in some cases.
This is especially true when it comes to neuropathy caused by alcoholism, vitamin deficiency, toxins, and certain medications. Implementing certain lifestyle changes can significantly improve the chances of recovery.
Of course, this isn’t always possible.
The good news is that our nerves (have amazing regenerative abilities, meaning, they are able to heal themselves. However, there is a limit to this power, and sometimes, if the damage is too severe, the nerves aren’t able to fully repair themselves. When this happens, it’s possible to slow down the progression of the disorder, but not completely reverse it.
The earlier you manage to diagnose your condition and seek treatment, the better chance you’ll have at recovery, however, the body is capable of many miraculous things, so always, I repeat…. always, remain hopeful.
Treatments for peripheral neuropathy depends on the cause of the condition. Some types of neuropathy may require medical intervention like surgery or injections, while others can be effectively treated through physical therapy and lifestyle modifications.
MEDICAL TREATMENTS
Surgery
Peripheral neuropathy caused by physical injury or nerve compression often requires surgical treatments. These procedures are called nerve decompression surgeries and their aim is to relieve the pressure caused by a pinched or entrapped nerve. This type of surgery is not overly invasive and is believed to be successful in 80% to 90% of cases.
Therapy
Several therapies can help ease the symptoms of neuropathy.
Physical therapy aims at treatments to reduce symptoms and improve muscle strength and mobility issues.
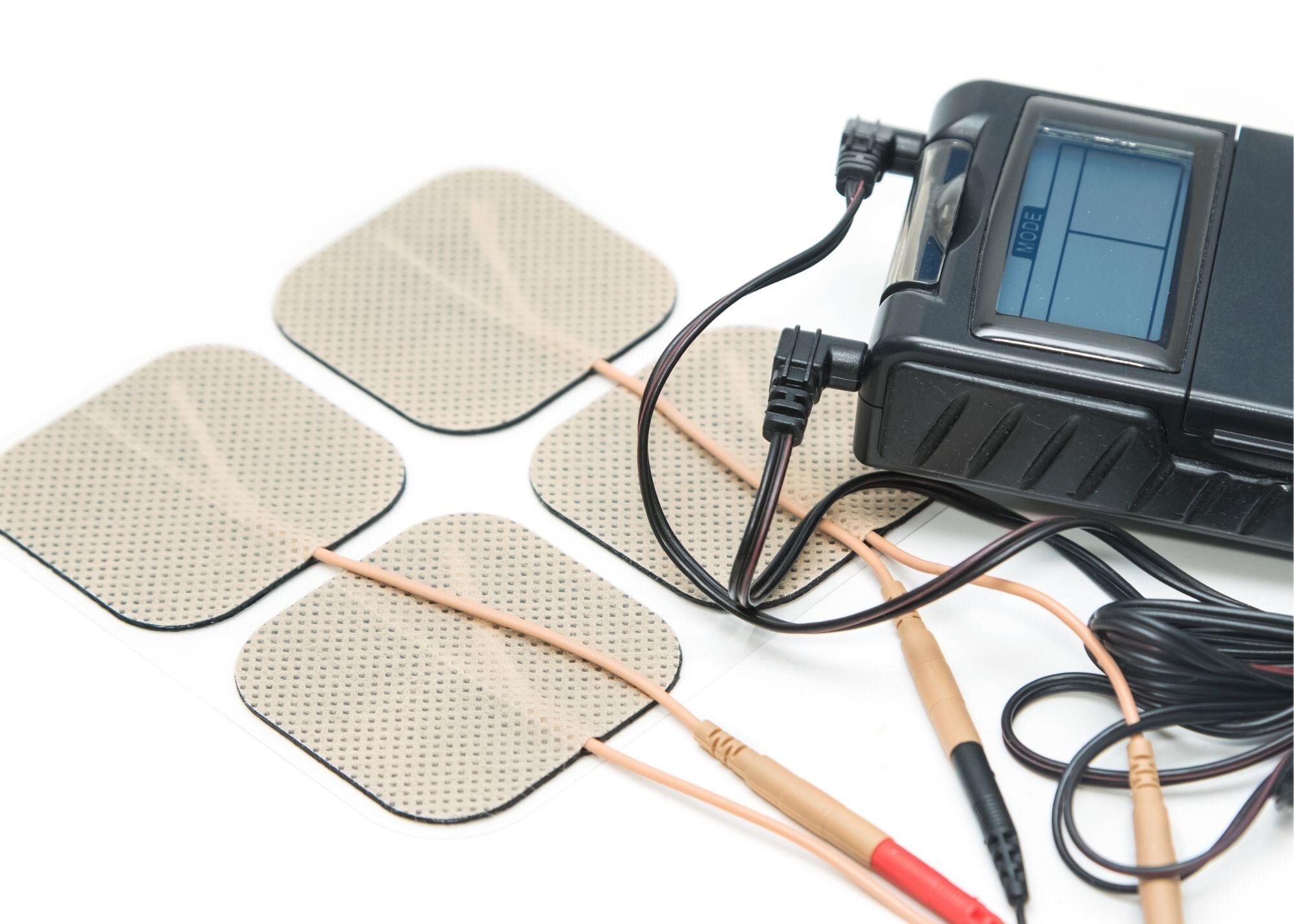
However, other, therapies like transcutaneous electrical nerve stimulation (TENS) plasma exchange (PE) and intravenous immune globulin (IVIg) have also proven to be effective tools for relieving the symptoms and signs of neuropathy.
TENS unit.
TENS therapy relies on electrical currents to stimulate the nerves. Studies show that TENS therapy can significantly decrease pain in patients suffering from neuropathy as well as other painful conditions. These devices are small units that can be self-administered and are not difficult to use. TENS units can be easily purchased online. I recommend you see your Doctor or Physiotherapist to determine if a TENS unit is suitable for you and they can also help show you how to use it appropriately
Medication
Easing the symptoms of peripheral neuropathy can also be achieved through the use of certain medications. Depending on the severity of the symptoms, your doctor may prescribe pain relievers, anti-seizure medications, and even antidepressants.
NATURAL TREATMENTS
Quitting Harmful Habits
The first step in improving your health and the symptoms associated with peripheral neuropathy is minimising exposure to, or stopping, substances that can be causing harm to your health.
We all know the damage smoking does to our health and it can limit the blood flow to your nerve cells, impairing your blood circulation in the process.
Additionally, alcohol abuse is linked to nerve damage and can even cause permanent disability in some cases.
The first step towards a successful recovery starts with making small, but effective modifications that can change your life for the better.
If this is an issue for you, speak to your doctor about the options you have available for this.
Diet
Get your Diet right! Start eating healthier.
Move away from processed food and do your best to start eating the best quality natural foods.
Eat foods that are high in nutrients and decrease or cut out anything that can be detrimental to your health.
This will help decrease the inflammation in your body and ensure you are getting all nutrients you need to support good health.(For more on healthy eating, check out more of my healthy eating articles HERE)
As mentioned earlier, certain types of neuropathy are directly caused by vitamin deficiencies, particularly certain vitamin B deficiency (mainly vitamin B-12).
Meat and dairy products are some of the best sources of B vitamins, which is why those following a plant-based diet are commonly at risk for deficiency.
It is possible to increase the intake of B vitamins through supplements, although it is necessary to consult with your doctor first to determine the right dosage and it is always best to get your nutrients from real food and only supplement if necessary.
Relaxation Technique
Anxiety, depression, chronic stress and worry all lead to a sensitised nervous system.
When you’re in a state of chronic stress (even mild) you are going to experience more pain and other symptoms.
Make lowering stress a priority in your life. When we are more relaxed, our nervous system is less sensitive, and symptoms will be reduced.
Lowering stress is a very important step towards recovery not only with peripheral neuropathy symptoms but your health in general, which is why it’s crucial to find a suitable way to decrease your stress levels.
Several techniques have proven to be effective in relieving stress and also pain caused by neuropathy.
Most of these methods rely on a body-mind connection, allowing you to ease symptoms of pain, but also help you cope with the condition.
Meditation, is very effective in reducing symptoms in not only peripheral neuropathy but also many other painful conditions.
Desensitisation Techniques
When sensation is increased in the hands or feet a light massage with moisturiser or cream of your choice can help reduce the symptoms.
Not only is massage good for sensitivity it will reduce pain, improve balance and improve range of motion also.
Another technique that may sound a bit crazy but is used frequently by Physiotherapists (which you can do yourself), is gently moving your hands or feet in a bucket of dry rice or dry beans. The texture of these items stimulates the nervous system and calms down the nerves.
Acupuncture
Another type of alternative medicine that relies on stimulating pressure points on the body. Through stimulation of the nervous system, the body releases endorphins, which act as natural painkillers.
Although not many people believe in the effectiveness of this technique, certain studies have confirmed the successfulness of acupuncture in treating neuropathic pain.
Exercise
Increasing activity levels can help combat the symptoms of neuropathy.
Regular exercise is beneficial for blood sugar control, as well as stress relief, both of which can greatly improve neuropathic pain.
Multiple studies have confirmed that routine exercise can prevent, and in some cases delay, the onset of neuropathic symptoms.
In the next section, we’ll go through some helpful exercises for peripheral neuropathy in some of the following chapters.
EXERCISE TO IMPROVE PERIPHERAL NEUROPATHY SYMPTOMS
Dealing with neuropathic pain can be uncomfortable, to say the least. When you’re dealing with these symptoms, exercise may feel like the last thing you feel like doing. And that’s ok. Sometimes you will just have to wait for symptoms to ease. However, maintaining a regular exercise schedule will do a great deal in managing and improving neuropathy symptoms.
It’s necessary to consult with your doctor before starting any type of exercise, and it is highly recommended you see a Physiotherapist to get a full assessment and an individualised exercise plan for you.
When exercising, if you notice that certain activities make your pain and symptoms worse, you should communicate this with your doctor or Physiotherapist.
Easing the symptoms of neuropathy can be achieved through an exercise program including aerobic exercise, exercises for flexibility and joint range of motion, balance and strengthening exercises, and exercises for pain management.
Aerobic exercises
Walking, swimming or cycling are some examples of great light aerobic exercises that can help you with neuropathic pain.
Undertaking aerobic exercises three times a week will improve your blood flow, work your muscles, and increase your heart and breathing rate. Improved fitness will help with pain and other symptoms.
Aim for 20-30 minutes of aerobic exercise per day. Always work your way up to this amount. Start with a few days per week at a smaller time frame and gradually building your way up.
If you’re able, a great place to go walking is on a beach or on soft grass. Being out in nature combined with the different textures of the sand or grass on your feet will help with symptoms whilst also getting the additional benefits of walking.
Stretching exercises
Flexibility exercises can help keep your joints flexible, which can, in return, improve your balance and minimise the risk of falls.
These types of exercises are also instrumental in preventing injuries during other activities. Incorporating static and dynamic stretches into your workout routines is the best way to ensure a safe and successful exercise outcome.
Balance exercises
Muscle weakness and numbness are common symptoms of peripheral neuropathy. This can greatly interfere with everyday life and can cause issues with balance and coordination.
Balancing exercises can help you improve your balance and proprioception and by doing this decrease your falls risk.
SPECIFIC EXERCISES FOR PERIPHERAL NEUROPATHY
The exercises below can help reduce your neuropathy symptoms by moving the area, improving blood flow to the area and relaxing the area.
Additionally, when range of motion/flexibility and strength are improved - pain and other symptoms (numbness/tingling etc.) will be reduced.
In the below exercises, we start with lower repetitions to ensure symptoms are not aggravated. Stay patient, and work your way up to more repetitions and sets over time.
WE START WITH LOWER REPETITIONS TO ENSURE WE DO NOT AGGRAVATE SYMPTOMS. STAY PATIENT.
SEATED PERIPHERAL NEUROPATHY EXERCISES FOR THE LOWER LEGS AND FEET.
TOE RAISES
Toe Raise Exercise
How To:
Place your feet flat on the floor.
Whilst the balls of your foot remains on the floor throughout, gently lift up your toes.
Hold for a few seconds and lower back to the ground.
Repeat for 5 Repetitions.
TOE SPLAYS
Toe Splays - Spreading Toes Apart - (I am not a good toe splayer :)
How To:
Place your feet flat on the floor
Now do your best to splay your toes (moving them apart).
Hold for a few seconds and relax your toes again.
Repeat for 5 repetitions.
TOE RAISES
Toes Raises
How To:
Place your feet flat on the floor.
Whilst only the heels of your foot remain on the floor throughout, gently lift up your toes and the rest of your foot.
Hold for a few seconds and lower back to the ground.
Repeat for 5 Repetitions.
HEEL RAISES
Heel Raises
ANKLE PUMPS
How To:
Place your feet flat on the floor.
Whilst only the balls of your feet and toes remain on the floor throughout, gently lift up your heels, and the rest of your foot.
Hold for a few seconds and lower back to the ground.
Repeat for 5 Repetitions.
Ankle Pumps
How To:
Sitting in your chair.
Pull your toes up toward you.
Now point your toes away from you.
Repeat for time/set repetitions.
KNEE EXTENSIONS
Knee Extensions
How To:
Sitting up tall with your shoulders back and down.
Lifting one leg up, extend at the knee.
Hold briefly at the top of the movement, squeezing the muscles at the front of the thigh before lowering your leg back down.
Ensure the movement is slow and controlled.
Repeat for 5 repetitions and repeat on the opposite leg.
SEATED HAMSTRING STRETCH
Hamstring Stretch
How To:
Shuffle to the front of your chair, place one leg in front of you, and sit up tall.
Now keep your leg straight and point your toes towards the ceiling
Ensure you remain upright with a straight back and lean slightly forward at the hips until you can feel a stretch in the back of your legs.
Hold for the set time and change legs.
SEATED CALF STRETCH (WiTH TOWEL)
Seated Calf Stretch
How To:
Shuffle to the front of your chair, place one leg in front of you, and sit up tall.
Now keep your leg straight and point your toes towards the ceiling.
Using a rolled-up towel, wrap the towel around the ball of your foot just below your toes.
Gently pull the towel towards you, allowing your foot to bend up slowly towards you. Keep your leg straight. You should feel a slight stretching feeling in the back of your lower leg.
Hold for the set time and change legs.
SEATED SOLEUS STRETCH (WITH TOWEL)
Seated Soleus Stretch
How To:
Shuffle to the front of your chair, place one leg in front of you, and sit up tall.
Now with a bend in your leg, point your toes towards the ceiling.
Using a rolled-up towel, wrap the towel around the ball of your foot just below your toes.
Gently pull the towel towards you, allowing your foot to bend up slowly towards you. You should feel a slight stretching feeling in the back of your lower leg.
Hold for the set time and change legs.
DESENSITISATION MASSAGE WITH MASSAGE BALL OR TENNIS BALL
Self Foot Massage
How To:
Place a massage ball (click here to purchase) or a tennis ball on the floor and whilst seated in a chair gently rub the sole of your foot over the ball. Make sure you get all areas.
This will help massage the foot muscles and stimulate the nervous system, calming the nerves.
Do this for 1-5 minutes and you can repeat this during the day.
STANDING PERIPHERAL NEUROPATHY EXERCISES FOR THE LOWER LEGS AND FEET.
CALF RAISES
Calf Raises
How To:
Stand up tall with your feet about hip-width apart.
Keep your knees straight and hold onto the chair with both hands.
Come up onto the toes, raise your heels up off the floor, hold briefly and slowly lower yourself back down.
Repeat for 5 repetitions.
TOE RAISES
Heel Raises
How To:
Stand up tall with your feet about hip-width apart.
Keep your knees straight and hold onto the chair with both hands.
Come up onto the heels, raise your toes up off the floor, hold briefly and slowly lower yourself back down.
Repeat for 5 repetitions.
HIP EXTENSIONS
How To:
Place both hands on your chair and stand up tall.
Keep your legs straight, slowly bring your leg back behind you, hold briefly and then bring your leg back to the start position.
Repeat for 5 repetitions and change legs.
HIP ABDUCTIONS
Hip Abductions
How To:
Stand tall holding on to your chair.
Slowly bring your leg out to the side and in a controlled motion bring your feet back together.
Ensure you keep your toes facing the front throughout this exercise.
Repeat for 5 repetitions and change legs.
KNEE FLEXIONS
Knee Flexion
How To:
Stand up tall, holding onto your chair.
Bend your leg at the knee, lifting your foot up towards your buttocks, to about 90 degrees, hold briefly and return your foot back to the start position.
Repeat for 5 repetitions and do the same on the opposite leg.
STANDING CALF STRETCH
Calf Stretch
How To:
Stand up tall, holding on to your chair with both hands.
Step one foot back, ensuring your toes are facing forward throughout the exercise.
Now bring your front knee towards the chair ensuring that your heels remain in contact with the floor at all times.
Hold this position for 30-60 seconds and change legs.
BALANCE - SEMI TANDEM STANCE, TANDEM STANCE OR SINGLE-LEG STANCE
Single Leg Stance Balance
How To:
Standing next to a chair for safety and stability.
Stand on one leg.
Hold this position for 30-60 seconds.
If you need to you can hold on with one or two hands on the chair.
You can make this exercise a little easier by standing in a semi-tandem or tandem stance position. Click here for balance positions.
Aim to increase your time in this position, without coming out of position, over time.
Relaxation - of the body - 2 Minutes
Spend at least two minutes a day focusing on relaxing your body. Sitting in silence. You can find relaxation videos in the app store on your phone or on YouTube. Also at the end of the video below, we go through a short relaxation sequence.
PERIPHERAL NEUROPATHY EXERCISE VIDEO FOR THE FEET & LEGS
A video you can follow to help with symptoms of peripheral neuropathy.
In this video, we go through seated and standing exercises including range of motion/flexibility/movement for pain relief, strengthening and balance. Plus it also covers self-massage/desensitisation and relaxation.
Exercises for neuropathy in feet and legs
PERIPHERAL NEUROPATHY EXERCISES FOR THE HANDS & ARMS
Exercises for neuropathy in hands and arms
MANAGING PERIPHERAL NEUROPATHY - TAKING PRECAUTIONS AT HOME
Peripheral neuropathy can have a great impact on your everyday life.
If you are suffering from this condition you are at a greater risk of accidents and injuries, when undertaking daily tasks.
There are certain precautions you can take to make your life safer while undergoing possible treatments for your condition.
Stop smoking and drinking alcohol, cut out unhealthy foods, and reduce stress.
Stay Active. You might be inclined to limit your activity levels due to muscle weakness and pain, but it’s important to keep active (without overdoing it). Aim to get moving more.
If symptoms of peripheral neuropathy are affecting your mobility and/or balance make sure you speak to your doctor or see a Physiotherapist so appropriate measures can be taken. You may need a walking aid.
If your balance is affected when walking, make sure to take your walking aid with you to reduce your risk of falls
Make sure to clear the paths around your house, to avoid tripping.
Wear well-fitted shoes at all times to help protect your feet from any injury, and make sure to regularly check your feet for cuts or sores that you may not have felt, especially after walking barefoot.
Take good care of your feet, trim your nails and see your Podiatrist as needed.
Avoid prolonged pressure on areas with nerve damage.
Keep your skin in good condition with a good moisturiser.
Shower and bath with caution. Avoid slips and falls by installing handrails in your bathroom and adding a non-slip mat on your bathroom floor. If you have a decreased sensitivity to touch, be careful when adjusting the water temperature when showering. Use your elbow to check the bathwater temperature before getting in.
Cook with caution. Again, if you have decreased sensitivity to touch, be mindful when dealing with hot objects in the kitchen at all times.
Pain and other symptoms associated with peripheral neuropathy are usually worse in colder climates. Keeping your hands and feet warm with a good set of gloves and socks can help reduce pain symptoms.